*Drs. Keshu Zhou, Mingyuan Sun, and Wei Xu are co-first authors; Drs. Jianyong Li, Jianxiang Wang, and Yifan Zhai are co-corresponding authors.
Introduction
Investigational lisaftoclax is a selective BCL-2 inhibitor that has demonstrated antileukemic activity and favorable tolerability in pts with CLL. We report updated efficacy and safety data of pts with CLL treated with lisaftoclax in phase 1b/2 studies APG-2575-CN001 (NCT03913949) and APG-2575-CC101 (NCT04494503) after a 14-month follow-up.
Methods
Lisaftoclax (100, 200, 400, 600, and 800 mg) was administered orally once daily to pts with relapsed/refractory (R/R) CLL in repeated 28-day cycles. A daily ramp-up schedule and close monitoring was used for prevention and early detection of tumor lysis syndrome (TLS). Lisaftoclax continued until disease progression, intolerable toxicity, death, or any other reason for termination. Adverse events (AEs) were reported per NCI CTCAE v5.0, and response was evaluated per 2008 iwCLL NCI-WG criteria. Flow cytometry was used to analyze minimal residual disease (MRD) at individual sites in pts who achieved complete response (CR)/CR with incomplete marrow recovery (CRi) and partial response (PR) based on investigator judgement. MRD negativity was defined as a threshold of < 10 -4.
Results
As of April 27, 2023, a total of 47 pts went through a daily ramp-up of lisaftoclax treatment at an assigned dose, ranging from 100 to 800 mg daily (100 [n = 3], 200 [2], 400 [12], 600 [14], and 800 [16] mg). The median (range) follow-up period was 14.06 (0.70-30.2) months, and the median (range) age was 58 (34-80) years (male, 68.1%), with an ECOG PS of 0-1. At enrollment, 53.2% of pts were in Rai stage III/IV, and 48.9% Binet stage C. A total of 66.0% and 44.7% of pts had been treated with ≥ 2 or 3 lines of systematic treatment, 23.4% > 1 Bruton tyrosine kinase (BTK) inhibitor, and 55.3% a CD20 antibody. A total of 36 (76.6%) pts experienced grade (Gr) 3/4 treatment-emergent AEs (TEAEs), and 13 (27.7%) had serious AEs (SAEs). Incidences of TEAEs were not dose related. Common (> 30%) TEAEs were decreased neutrophil (all Gr, 72.3%; Gr 3/4, 44.7%), platelet (all Gr, 59.6%; Gr 3/4, 31.9%), and leukocyte (all Gr, 51.1%; Gr 3/4, 14.9%) counts; anemia (all Gr, 48.9%; Gr 3/4, 10.6%); hypertriglyceridemia (all Gr, 44.7%; Gr 3/4, 4.3%); hyperuricemia (all Gr, 42.6%); hypokalemia (all Gr, 34.0%); diarrhea (all Gr, 34.0%); and hyperbilirubinemia (all Gr, 31.9%). TRAEs were observed in 45 (95.7%) pts, of whom 32 (68.1%) experienced Gr 3/4 AEs and 7 (14.9%) SAEs. One TLS was reported. Thirty-two (68.1%) pts discontinued the study due to disease progression (51.1%); withdrawal (6.4%); and AEs, investigator decision, poor compliance, protocol deviation, and other reasons (2.1% each).
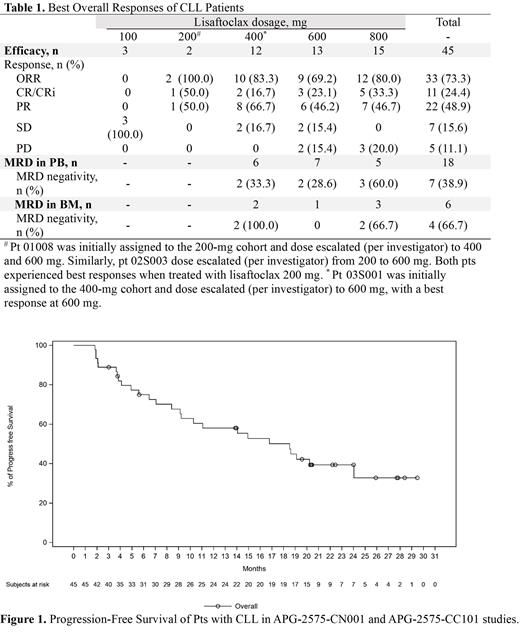
The median (range) time to first response was 2.07 (1.94-3.94) months. The overall response rate (ORR) was 73.3% (33/45), and the CR/CRi rate was 24.4% (11/45). The rate of CR/CRi seemed to be dose-dependent (16.7% at 400, 23.1% at 600, and 33.3% at 800 mg). Furthermore, the pt who achieved a CR in the 200-mg cohort showed systemic exposure (C max and AUC) to lisaftoclax comparable to that observed in the 600-mg cohort. One patient in the 400-mg cohort achieved a CR in response to a dose escalation (per investigator) to 600 mg. MRD negativity was observed in 7 of 18 (38.9%) pts tested with peripheral blood (PB) MRD assessment, and 4 of 6 (66.7%) pts tested negative for MRD with MRD assessment of bone marrow (BM; Table 1). Median progression-free survival (PFS) was 18.53 (95% CI, 9.13-24.05) months, and 12- and 24-month PFS rates were 58.0% (95% CI, 41.9-71.2) and 39.4% (95% CI, 24.4- 54.0), respectively, as shown in Figure 1. The median (range) duration of response was 20.24 (95% CI, 14.75-NR) months. Median overall survival (OS) was NR. OS at 12 and 30 months was 94.8% (95% CI 80.6-98.7) and 86.3% (95% CI 66.1-94.9), respectively.
Conclusions
Lisaftoclax demonstrated significant efficacy at 400, 600, and 800 mg, and potentially 200 mg, in pts with R/R CLL who were heavily pretreated and had been exposed to BTK inhibitors. CR/CRi exhibited a trend of positive correlation with escalating dose levels. No significant new or unmanageable safety findings were observed.
Disclosures
Chen:Ascentage Pharma: Current Employment, Current equity holder in publicly-traded company. Men:Ascentage Pharma: Current Employment, Current equity holder in publicly-traded company. Wang:Ascentage Pharma: Current Employment, Current equity holder in publicly-traded company. Zhang:Ascentage Pharma: Current Employment, Current holder of stock options in a privately-held company. Xu:Ascentage Pharma: Current Employment, Current holder of stock options in a privately-held company. Zhang:Ascentage Pharma: Current Employment, Current holder of stock options in a privately-held company. Yang:Ascentage Pharma: Current Employment, Current equity holder in publicly-traded company, Membership on an entity's Board of Directors or advisory committees, Other: Leadership, Patents & Royalties. Zhai:Ascentage Pharma: Current Employment, Current equity holder in publicly-traded company, Other: Leadership (CMO).

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal